Innovative Approaches for Teaching Clinically-Relevant Anatomy Utilizing Virtual Dissection Software
Anyone who has ever been assigned to teach a course in human anatomy knows that doing so is a daunting task. The breadth of the topic is enormous and yet any discussion solely dedicated to anatomy and devoid of any mention of associated physiological and/or clinical information will be unimaginably tedious and virtually devoid of any value. As such, the instructor is forced to make many important decisions regarding the degree to which anatomical, physiological, and clinical topics can be blended to ultimately yield a course that is both manageable in the time allowed and worthwhile. In addition, anatomy is a highly visual, three-dimensional discipline, so instructors must skillfully balance the options available to present such information (e.g., computer programs, models, cadavers) with the educational needs of the students and the physical and financial resources of the institution. This article will further elucidate some of these challenges and suggest a variety of solutions to overcome them.
Managing Content
According to Bartleby.com, Grey's textbook of anatomy addresses in 13,000 anatomic structures ranging from the Antrum of Highmore to the Zonule of Zinn. Given that most introductory courses in anatomy are likely going to be assigned 3-5 credit hours, the instructor must swiftly turn attention to whittling the structure list down to a level of content that can be managed in the time allotted. Recognizing that the vast majority of students enrolled in undergraduate human anatomy courses have aspirations to enter the health-care field, it is prudent to let these aspirations guide decisions regarding which structures must be emphasized, which can be given less attention, and which can, in all likelihood, be safely ignored altogether. Of course, this task becomes even easier if the career goals of the students in the class are the same or similar. For example, a student hoping to become a massage therapist will definitely require an emphasis on muscular, skeletal, and neurologic structures, while discussions focused in these areas will be substantially less useful for those destined for a career in pharmacy.
Of course, for the instructor to make content decisions based on clinical expectations, he or she must have at least some degree of clinical experience or have someone or something (e.g., a textbook) that can offer a clinical spin on anatomical concepts available for consultation. If this is not possible, or if the career goals of the students in the class are quite diverse, content selections may have to be based on the answer to the question, "What would be the consequence to a person if this structure were to fail?" Obviously, those structures for which failure would more likely and most directly result in loss of life, limb, or significant function would rise to the top of the list of structures that should be included in the course content, as would the primary blood and nervous supply to these structures.
Including Physiology
Technically, pointing out and naming structures in an atlas or on a cadaver constitutes teaching anatomy, albeit to an extremelylimited degree. Even going a step further by saying such things as, "The pelvic bone is connected to the thigh bone and the thigh bone is connected to the knee bone," yields only marginally more useful information. The point is that teaching anatomy alone, without including at least some instruction in physiology, is an unfulfilling exercise. As soon as students are told what a structure is and perhaps how it is constructed (i.e., the anatomy), they will want to know what it does (i.e., its physiology), and successful courses will have to incorporate both anatomic and physiologic information.
Unfortunately, even courses that contain both information about what structures are andwhat they do are at risk of being presented as lectures of lists, which, of course, does not optimally use lecture time. I have found that combining screenshots from the Animated Dissection of Anatomy for Medicine (ADAM) software program at various levels of depth, and combining these images with physiologic information available online into a series of PowerPoint presentations yields a set of electronic anatomy and physiology flashcards that allows students to learn the basics of anatomy and physiology on their own time or as part of a virtual lab. This leaves lecture time available for expansion upon the basic material, with discussions of clinical scenarios, for example, as described in the next section. The screenshot below from a presentation at the League's 2012 STEMtech conference illustrates how efficiently regional, systemic, and physiologic information can be arranged for student review. While it is very time consuming to initially set up these three-slide series for multiple structures at a particular level and then to repeat this process for multiple levels throughout the various body regions, it is well worth the investment.
Figure 1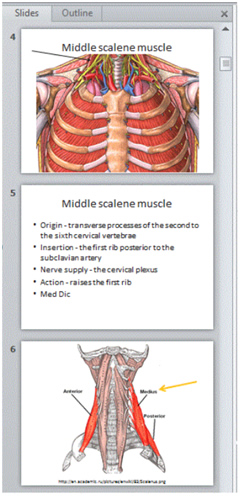
Used with permission
Figure 1 shows a screenshot of three slides within the PowerPoint file entitled Anterior Chest Level 146, demonstrating a highly succinct review of the regional anatomy, physiology, and systemic (i.e., musculoskeletal) anatomy of the middle scalene muscle. The number 146 refers to the depth at which this structure is located using the A.D.A.M. software program. The information on slide 5 was taken from The Free Dictionary by Farlex at http://www.thefreedictionary.com/ and the regional anatomy on slide 6 was copied from a free internet source entitled Academic Dictionaries and Encyclopedias at http://en.academic.ru/pictures/enwiki/83/Scalenus.png.
Including Clinical Scenarios
As mentioned earlier, most of the students taking an anatomy course are likely to be pursuing a career in health care, which means that they will have an inherent interest in the content of an anatomy and physiology course. However, this interest can be markedly enhanced and the overall effectiveness of the course greatly improved by tying the anatomic and physiologic information directly to realistic, clinical scenarios. Starting with real and common anatomically based clinical problems that can pull together important anatomical concepts (e.g., Bell's palsy, Horner's syndrome, pulmonary embolism) and working backward to identify the basic anatomy most relevant to these conditions can be a very interesting and rewarding exercise for faculty and students alike.
Of course, as noted earlier, the degree to which clinical scenarios can be effectively identified and incorporated into lectures is limited by the clinical experience of the instructor and the amount of time available for instruction. On the other hand, identifying the clinical states the students in the class are most likely to see once they become clinicians and the most relevant anatomy associated with these conditions can help the instructor truncate the amount of basic material to be taught and can actually help create time for the presentation of clinical scenarios.
Including Regional Anatomy
Many introductory courses in anatomy are taught in a systemic format. That is, topic areas are divided by systems (e.g., circulatory, respiratory, digestive). This format works well from a general education standpoint, but for pre-clinical students, the instructor might want to consider a regional format outright, or at least consider incorporating some regional discussions in an otherwise systemic course. The reason that regional anatomy (i.e., the simultaneous consideration of all of the anatomical structures in an area of the body and the interrelationships of these structures) is important is that patients often present with regional complaints (e.g., chest pain, abdominal pain, ankle pain) that can represent problems in structures from multiple systems. For example, the source of pain in a patient with chest discomfort may be within the musculoskeletal structures of the chest wall, the heart, the lungs, and/or the esophagus. Recalling that the ribs lie anterior to the other structures of the chest, the clinician can reason that if palpation of the chest augments the pain, it is likely that the patient is not having a heart attack or suffering from gastroesophageal reflux, but is the victim of some musculoskeletal abnormality. While this is a fairly obvious example, it does illustrate how regional anatomy can be directly applied to practice while systemic anatomy taught in systemic vacuums can limit the clinician's capacity for critical thinking.
One technique used to incorporate regional anatomy into an almost exclusively systemic course is to periodically assign groups of students to prepare a presentation in which they are asked to track the course of some type of penetrating object (e.g., a knife or bullet) through various regions of the body and then report to the class what the clinical consequences would likely be as various structures (each progressively more deeply situated than the last) are damaged. I found that the A.D.A.M. software program is very well suited to this type of project, providing a very easy way for students to investigate multiple levels of penetration and to identify the structures and their interrelationships at these levels.
Making the Material Accessible in Multiple Locations
One common lament that is heard from clinicians is that they wish they could be re-exposed to anatomical instruction after they have gained some clinical experience. The feeling is that with clinical experience, the anatomic information originally presented would be easier to remember, seem more relevant, and ultimately help them make better decisions in the clinical setting. As it turns out, the same concise information provided in Figure 1 above can be easily viewed on mobile devices, such as the iPad, and therefore be readily accessible for use in clinical environments. When these files are grouped by dissection depth and then maintained in folders identified by body area (the screenshot in Figure 2 below shows the contents of the Anterior Chest folder), it is easy for the clinician or clinical student to quickly review regional anatomy at various depths while evaluating a wound, interpreting a CT scan, or observing the progress of a surgery. Such a review can refresh and/or build the clinician's clinically-relevant, anatomic knowledge base and lessen the likelihood of anatomically-related oversights when considering diagnostic possibilities or planning procedures.
Figure 2
Used with permission
Figure 2 is a screenshot of the contents of the entire Anterior Chest folder. Eighteen depths of dissection were deemed to be particularly important for review (labeled 2-270). Each of the individual files contain a series of two to three slides containing the information shown in Figure 1 above for each of the structures visible at the designated depth level (e.g., 2, 10, 21).
Summary
There are many demands on instructors of anatomy courses, including: (1) selecting the appropriate mix of basic anatomy, physiology, clinical scenarios, and regional anatomy that will meet the needs of the students; (2) ensuring that this material will be teachable within the time allotted and with the resources available; and (3) getting all of this done in a format that will be conveniently available to the students not only during the course but in their future practice settings. Strategies to meet these challenges were discussed. The concept that anatomical structures are not equivalent in their clinical significance was developed as was a method for applying this concept to help reduce the overall amount of basic anatomical content in a course to make room for discussions of physiology and clinical scenarios. The importance of including regional anatomy, a strategy to accomplish this, and its capacity to augment clinical performance and develop critical thinking was identified. Finally, the advantages and method of providing this information in a mobile, electronic format was highlighted.
John A. Lucich, M.D., is chair of the Admissions Committee for the Physician Assistant Program at Butler University in Indianapolis, Indiana. This article is based on a presentation he made at the League's STEMtech Conference in October 2012.
Opinions expressed in Innovation Showcase are those of the author and do not necessarily represent those of the League for Innovation in the Community College










